Current issues include:
Advocating against cuts to the NIH budget:
In 2019, NIH funded 5,681 projects in New York State, totaling $2.89 billion; 68% of which supported research at our medical schools. These funds are instrumental in driving both discoveries and economic activity in our state. President Trump has proposed draconian cuts to the NIH budget that would prove devastating to New York State’s biomedical research community. Read more about NIH awards here.
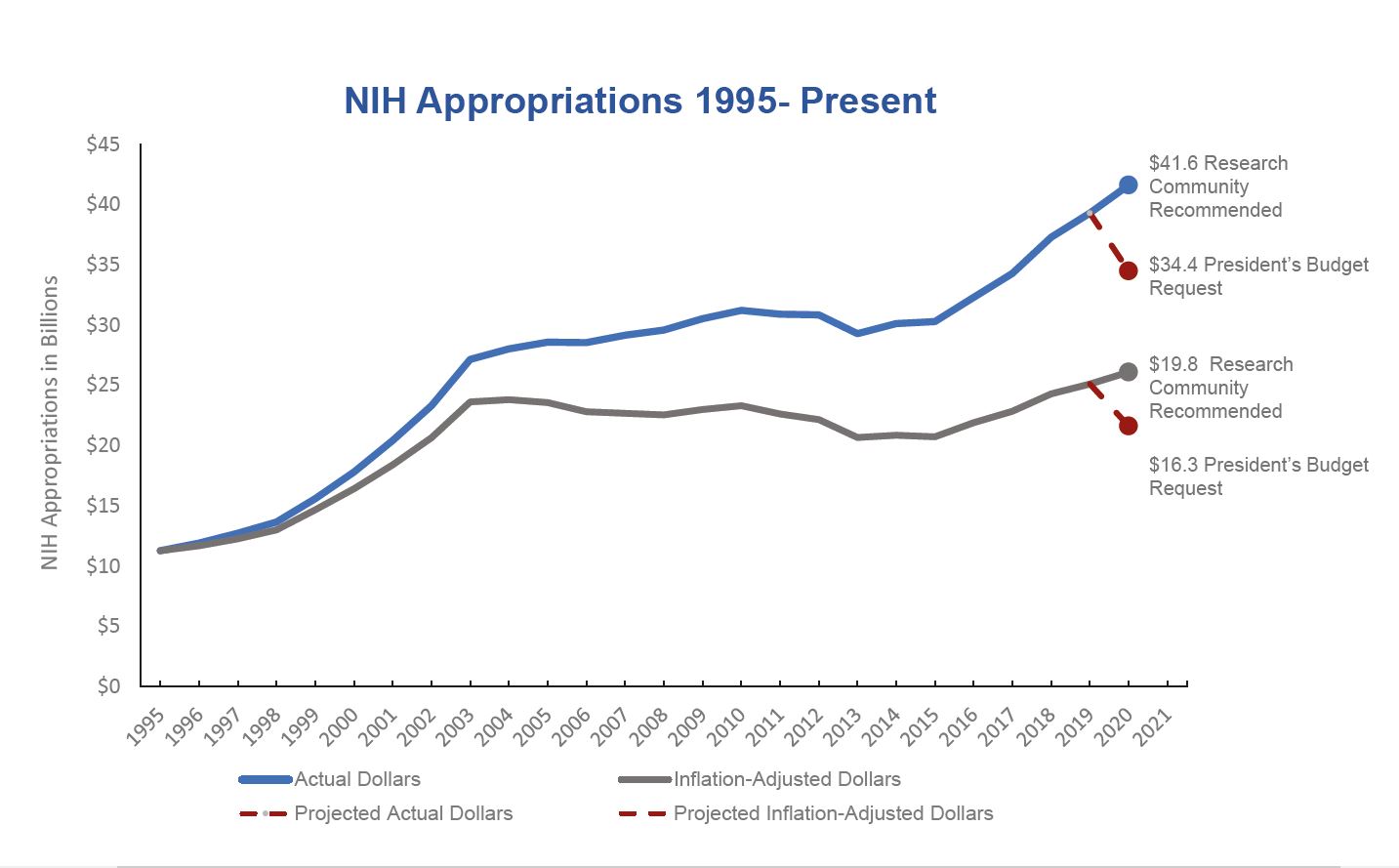 Sources: NIH Office of Budget, Appropriations History, Price Indexes, Budget Request, and FASEB Annual Federal Funding Recommendations
Sources: NIH Office of Budget, Appropriations History, Price Indexes, Budget Request, and FASEB Annual Federal Funding Recommendations
Policy Positions:
AMSNY Letter of Endorsement for H.R. 8049 The Dr. Lorna Breen Health Care Provider Protection Act of 2020 and S.4349 The Dr. Lorna Breen Health Care Provider Protection Act of 2020
